Introduction:
Once iodine enters your body—whether through food, water, or supplements—it begins a complex and highly regulated journey. From the digestive system to the thyroid gland, every step of iodine’s path is finely tuned to support hormone production without tipping into excess. In this article, we’ll explore how your body absorbs iodine, how it uses and stores it, and what can influence how much of that iodine is actually available to your cells.
Iodine Enters Through the Digestive Tract
Most dietary iodine comes in the form of iodide (I⁻), a soluble and easily absorbable form of iodine. Once you consume iodine-containing foods, it is absorbed:
- Primarily in the stomach and upper small intestine
- Very efficiently — about 90% of dietary iodide is absorbed
From there, iodide enters the bloodstream and is rapidly taken up by various tissues—especially the thyroid gland, which uses it to produce hormones.
The Thyroid: Iodine’s Main Destination
The thyroid gland is the body’s iodine reservoir. It absorbs iodine from the blood through a specialized transporter called the sodium-iodide symporter (NIS).
Inside the thyroid:
- Iodide is oxidized and bound to the amino acid tyrosine.
- These modified tyrosines combine to form T3 and T4, the body’s primary thyroid hormones.
The gland stores several weeks’ worth of iodine, giving it a buffer against short-term fluctuations in intake.
Regulation by TSH (Thyroid-Stimulating Hormone)
Iodine absorption and use are controlled by the thyroid-pituitary feedback loop:
- The pituitary gland releases TSH (thyroid-stimulating hormone).
- TSH signals the thyroid to absorb more iodine and make more hormones.
- When T3 and T4 levels are sufficient, TSH production decreases.
- When levels drop, TSH increases, pushing the thyroid to absorb more iodine again.
This feedback loop keeps iodine use responsive and adaptable, helping your body adjust to your metabolic needs.
Factors That Affect Iodine Bioavailability
While iodine is generally well absorbed, several factors can influence how much is actually usable in the body:
Nutrient Interactions:
- Selenium is essential for converting T4 into the more active T3.
- Iron deficiency can impair thyroid function and lower iodine efficiency.
- Zinc supports the production of TSH.
Dietary Inhibitors (Goitrogens):
Certain compounds can block iodine uptake by the thyroid, especially when iodine intake is already low. These are found in:
- Cruciferous vegetables (cabbage, kale, broccoli)
- Cassava
- Soy-based foods
Note: Cooking these foods significantly reduces their goitrogenic effects. For most people with adequate iodine intake, these foods do not pose a problem.
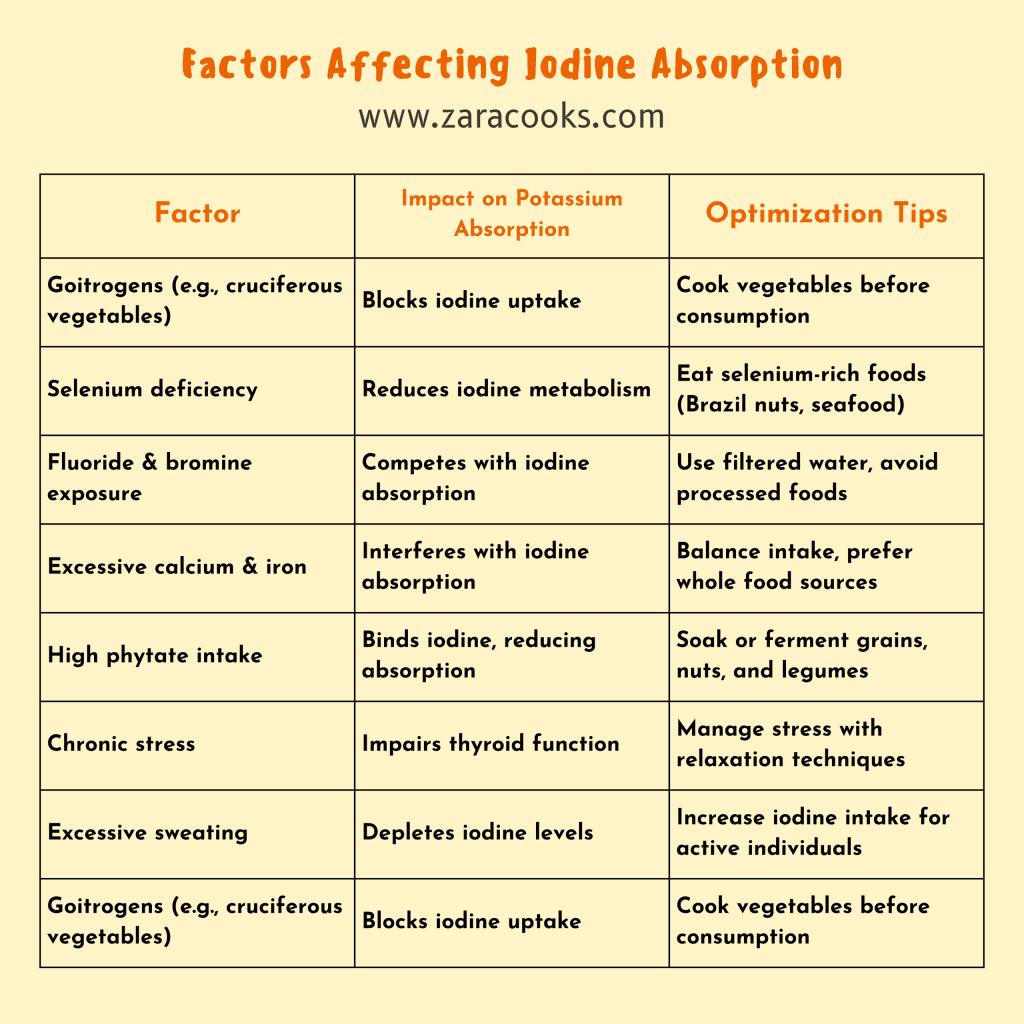
Environmental and Lifestyle Factors
- Soil iodine levels: Populations in iodine-poor regions are more likely to have deficiencies, especially where food isn’t fortified.
- High nitrate exposure (from drinking water or fertilizer) may interfere with iodine uptake.
- Smoking: Contains thiocyanate, which competes with iodine for uptake in the thyroid.
Pregnancy and lactation: Increase the body’s iodine requirement due to higher hormone production and fetal development needs.
Summary Table: Iodine Absorption and Influencers
| Step | What Happens |
| Absorption | Iodide absorbed efficiently in the stomach and small intestine |
| Transport | Carried in blood to the thyroid via the sodium-iodide symporter |
| Use | Converted into thyroid hormones (T3 & T4) |
| Regulation | Controlled by TSH from the pituitary gland |
| Influencing Nutrients | Selenium, iron, and zinc support iodine metabolism |
| Inhibitors | Goitrogens (in some foods), smoking, nitrates |
| Increased Needs | Pregnancy, lactation, and certain medical conditions |
Conclusion:
Iodine’s story doesn’t end with absorption—it’s how it interacts with the rest of the nutrient ecosystem and lifestyle choices that truly shapes its impact. In the final article of this series, we’ll dive into the top iodine-rich foods, both animal and plant-based, and how to meet your needs without going overboard.